The Latest Breakthroughs in Alzheimer Treatment You Should Know About
Recent advancements in Alzheimer's disease research have opened promising avenues for treatment, offering hope to millions affected worldwide. From novel drug therapies targeting amyloid plaques to innovative non-pharmacological approaches, the landscape of Alzheimer treatment continues to evolve rapidly. Understanding these breakthroughs is essential for patients, caregivers, and healthcare providers navigating this challenging condition.

Alzheimer’s disease affects approximately 6.5 million Americans aged 65 and older, with numbers expected to rise significantly in the coming years. As researchers deepen their understanding of the disease mechanisms, treatment approaches are becoming more sophisticated and targeted. Recent breakthroughs offer new possibilities for managing symptoms, slowing progression, and potentially altering the course of this devastating neurodegenerative condition.
Anticipated Alzheimer Treatment Developments for 2025
The coming years hold significant promise for Alzheimer’s treatment. Several therapies currently in late-stage clinical trials may receive approval by 2025, potentially expanding the treatment arsenal. Among these are monoclonal antibodies that target toxic protein accumulations in the brain. Following the FDA’s approval of lecanemab (Leqembi) and donanemab’s promising phase 3 results, several similar drugs are advancing through clinical pipelines.
Beyond amyloid-targeting therapies, treatments focusing on tau protein, neuroinflammation, and metabolic factors are showing potential. Combination therapies—utilizing multiple mechanisms simultaneously—represent another frontier expected to gain traction by 2025. Additionally, precision medicine approaches using genetic biomarkers to personalize treatment plans are anticipated to become more widely implemented, allowing for more targeted interventions based on individual disease characteristics.
Understanding Alzheimer Treatment Costs
The financial burden of Alzheimer’s treatment represents a significant challenge for patients and families. Current FDA-approved medications vary considerably in price, with newer monoclonal antibody treatments being particularly expensive. For instance, lecanemab (Leqembi) costs approximately $26,500 annually before insurance, while traditional symptom-managing medications like donepezil may cost between $30 and $200 monthly depending on dosage and formulation.
Beyond medication expenses, comprehensive Alzheimer’s care includes diagnostic testing, regular physician visits, potential hospitalizations, and long-term care costs. Diagnostic procedures such as PET scans can cost $3,000-$6,000, while specialized memory care facilities average $5,000-$8,000 monthly. Medicare coverage for newer treatments remains limited, with Part B covering some treatments under specific circumstances, while many private insurers require extensive documentation before approving coverage.
Alzheimer Treatment Comparison: Approaches and Efficacy
Current Alzheimer’s treatments fall into several categories, each with distinct mechanisms and efficacy profiles. Cholinesterase inhibitors (donepezil, rivastigmine, galantamine) work by increasing acetylcholine levels in the brain, typically offering modest symptomatic improvement in memory and thinking. NMDA receptor antagonists like memantine regulate glutamate activity, sometimes used in combination with cholinesterase inhibitors for moderate to severe stages.
The newer class of amyloid-targeting therapies represents a shift toward disease modification rather than symptom management. Lecanemab has demonstrated ability to reduce amyloid plaques and slow cognitive decline by approximately 27% in clinical trials, though with potential side effects including amyloid-related imaging abnormalities (ARIA). Non-pharmacological approaches, including cognitive stimulation therapy, physical exercise programs, and dietary interventions, show varying degrees of benefit for symptom management and quality of life, often with fewer adverse effects than medications.
Navigating Alzheimer Treatment Prices and Insurance Coverage
The financial landscape of Alzheimer’s treatment is complex and varies significantly based on treatment type, insurance coverage, and geographic location. Out-of-pocket expenses depend heavily on insurance plans, with Medicare Part D covering many traditional medications but imposing significant restrictions on newer therapies. Medicare beneficiaries may face annual out-of-pocket costs ranging from several hundred to several thousand dollars for comprehensive treatment.
For the latest amyloid-targeting therapies, coverage remains inconsistent. Medicare has implemented coverage with evidence development (CED) programs for monoclonal antibody treatments, requiring participation in approved studies for coverage. Patient assistance programs from pharmaceutical manufacturers can help reduce costs, with some programs covering up to 20% of the medication cost for eligible patients. Additionally, nonprofit organizations like the Alzheimer’s Association offer grant programs to help offset treatment expenses for qualified individuals.
Comparison of Current FDA-Approved Alzheimer Treatments
| Treatment | Mechanism | Average Annual Cost | Potential Benefits | Common Side Effects |
|---|---|---|---|---|
| Donepezil (Aricept) | Cholinesterase inhibitor | $1,200-$4,000 | Modest improvement in memory and cognition | Nausea, diarrhea, insomnia |
| Memantine (Namenda) | NMDA receptor antagonist | $3,000-$5,000 | Moderate improvement in cognitive function | Dizziness, headache, confusion |
| Rivastigmine (Exelon) | Cholinesterase inhibitor | $2,400-$6,000 | Slight improvement in daily functioning | GI distress, decreased appetite |
| Lecanemab (Leqembi) | Anti-amyloid antibody | $26,500 | 27% slower disease progression | ARIA, infusion reactions |
| Aducanumab (Aduhelm) | Anti-amyloid antibody | $28,200 | Reduction in amyloid plaques | ARIA, headache, falls |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Emerging Non-Pharmacological Alzheimer Treatments
Beyond medications, innovative non-pharmacological approaches are gaining recognition for their potential benefits in Alzheimer’s care. Cognitive stimulation therapy programs, structured around themed activities to engage multiple cognitive domains, have shown improvements in quality of life and communication skills. Digital therapeutic interventions, including virtual reality environments and specialized cognitive training applications, offer accessible options for home-based cognitive maintenance.
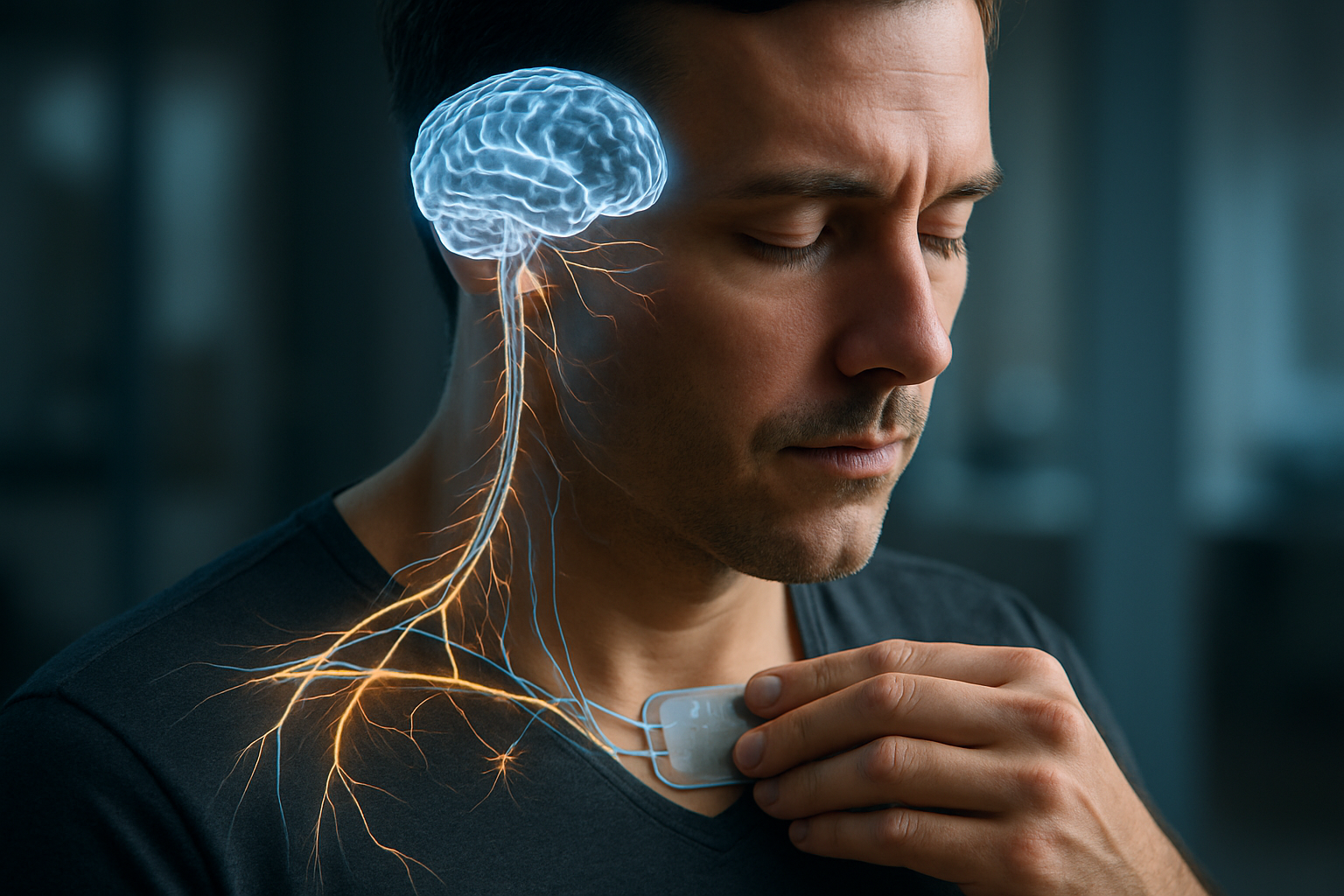
Transcranial magnetic stimulation (TMS) and focused ultrasound technologies represent emerging non-invasive neuromodulation techniques being investigated for their potential to improve cognitive function. Lifestyle interventions, particularly the MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) and structured exercise programs, have demonstrated potential preventive benefits and may complement pharmacological treatments. These approaches often carry fewer risks than medications and can be tailored to individual preferences and capabilities.
Alzheimer’s treatment continues to evolve rapidly, with promising developments on multiple fronts. From disease-modifying antibodies to innovative non-pharmacological approaches, the treatment landscape offers more options than ever before. While significant challenges remain—including high costs, side effect profiles, and variable insurance coverage—ongoing research provides hope for more effective, accessible treatments in the coming years. Patients and families navigating Alzheimer’s disease should work closely with healthcare providers to develop comprehensive treatment plans that address both the neurological aspects of the disease and the broader impacts on daily functioning and quality of life.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.